Once the elbow is hurt, you have to keep up preventive/active treatments as long as you play! Stiff frames, high string tensions, off center shots can torque out the elbow and cause injury. Golfers also hurt the elbow, as do electricians, turning screw drivers and using hole hawg drills.
The flex bar works well. http://hubpages.com/hub/Flexbar-The-...t-Tennis-Elbow http://the-therapy-connection.com/B0...B000P7YMW0.htm
The tenex impact absorber works for prevention: http://www.tenniscompany.com/accessory_Tenex.html http://www.tennis-elbow.com/
Also, right here in Montclair, Ice compression/velcro: http://www.petesice.com http://www.petesice.com/products.html
http://www2.massgeneral.org/sports/protocols.html Also has shoulder protocols.
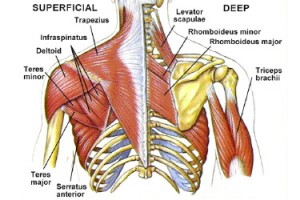
Rotator cuff:
http://www.youtube.com/watch?v=lTRvx...eature=related rotator cuff
http://www.eorthopod.com/content/sur...tation-program rotator cuff
plantar fasciitis and other foot injuries: shoes http://well.blogs.nytimes.com/2010/0...vent-injuries/
wrist injuries: http://www.eorthopod.com/content/tri...-tfcc-injuries
http://www.youtube.com/watch?v=3F3ovb2kZ9Q chi master
cHI ENERGY MASTER: HEALING INJURY
The flex bar works well. http://hubpages.com/hub/Flexbar-The-...t-Tennis-Elbow http://the-therapy-connection.com/B0...B000P7YMW0.htm
The tenex impact absorber works for prevention: http://www.tenniscompany.com/accessory_Tenex.html http://www.tennis-elbow.com/
Also, right here in Montclair, Ice compression/velcro: http://www.petesice.com http://www.petesice.com/products.html
http://www2.massgeneral.org/sports/protocols.html Also has shoulder protocols.
Rotator cuff:
http://www.youtube.com/watch?v=lTRvx...eature=related rotator cuff
http://www.eorthopod.com/content/sur...tation-program rotator cuff
plantar fasciitis and other foot injuries: shoes http://well.blogs.nytimes.com/2010/0...vent-injuries/
wrist injuries: http://www.eorthopod.com/content/tri...-tfcc-injuries
http://www.youtube.com/watch?v=3F3ovb2kZ9Q chi master
cHI ENERGY MASTER: HEALING INJURY



Comment